Reflux
What is Reflux?
Gastroesophageal reflux, also called acid reflux, occurs when food or acid from the stomach flows backward up into the esophagus and occasionally into the throat, mouth, and nose.
Some studies report that up to 30% of children with autism experience reflux. It is commonly misdiagnosed, underdiagnosed, or hard to diagnose in children with autism.
It is common to have occasional reflux from time to time, but reflux that happens too often can cause poor growth, vomiting, or chronic inflammation of the esophagus.
The lower esophageal sphincter (LES) is a ring of muscle that controls the opening between the esophagus and stomach. [6]
Reflux happens when the LES muscle relaxes at the wrong time or doesn’t close as it should.
Reflux is diagnosed through several methods including [6]:
Barium swallow test
Upper endoscopy
24 hour esophageal pH
Esophageal motility study
In children with autism, gastrointestinal symptoms such as reflux are common.
Reflux is commonly misdiagnosed, underdiagnosed or hard to diagnose in children with autism.
One study reported that up to 30%of children with autism experienced gastroesophageal reflux. [7]
Many common behaviors such as excessive chewing, regurgitation, or prolonged eating linked to reflux could be overlooked as OCD or developmental or structural concerns.
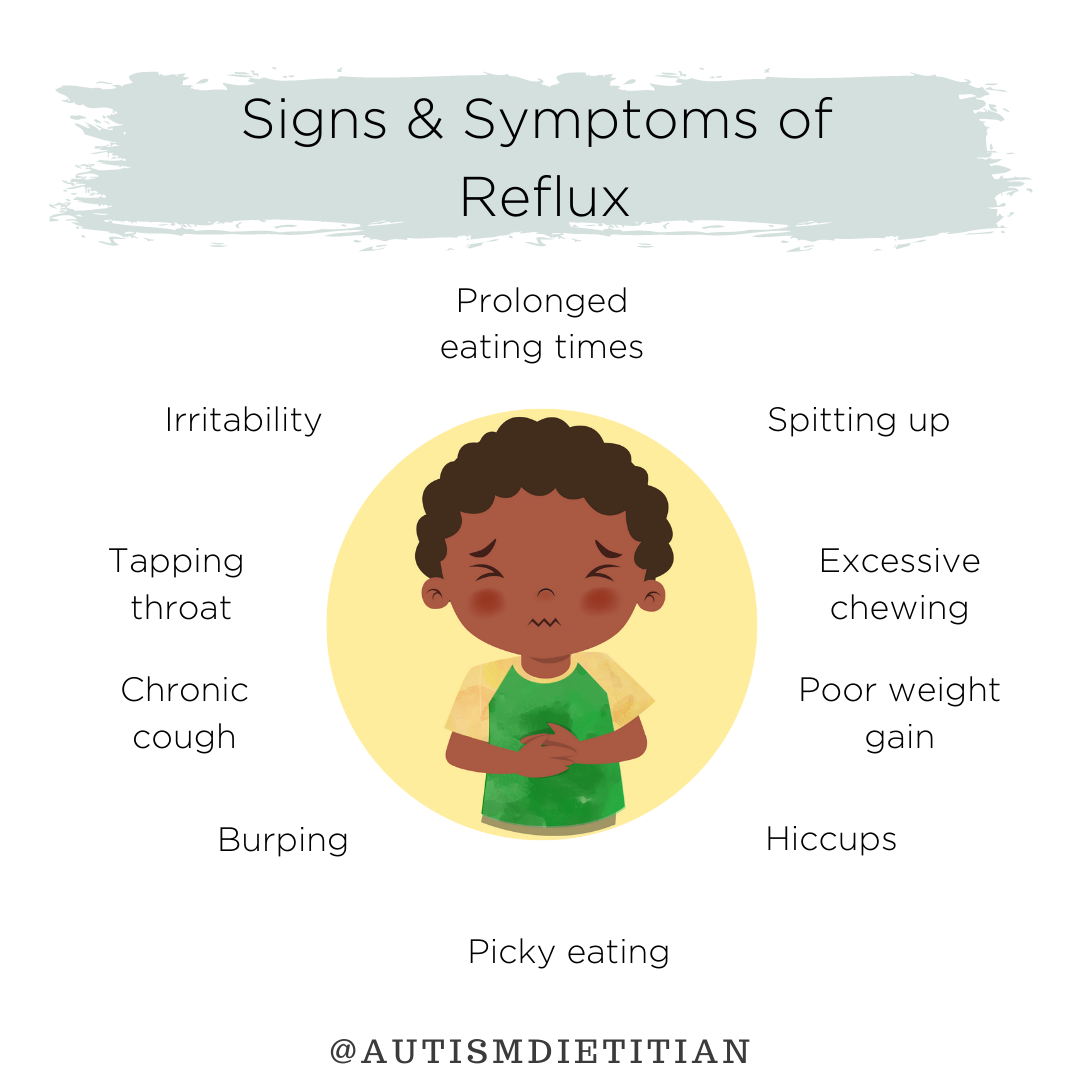
Source: Autism Dietitian Instagram
Signs/Symptoms
Regurgitation
Vomiting
Spitting-up
Heartburn/Chest pain
Backwashing
Child straining their neck or pushing out jaw
Child tapping their throat or chest
Constantly clearing the throat
Excessive chewing
Prolonged eating times
Difficulty swallowing
Frequent burping
Hiccups
Chronic cough or wheezing that doesn’t respond to asthma medications
Irritability and self-injurious behavior
Particularly during or shortly after eating
Poor weight gain
Halitosis (bad breath)
Damaged dental enamel
Potential Root Causes
Increased abdominal pressure related to:
Overweight/obesity
Gas and bloating
Low stomach acid production
Imbalanced gut bacteria
High intakes of fatty and fried foods
Underlying food sensitivities
Certain medications such as antidepressants, antihistamines, asthma medicines, sedatives, and pain relievers.
Helicobacter pylori infection
Hiatal Hernia
Next Steps
Nutritional Considerations for Reflux
Limit common foods that can cause reflux such as tomatoes, tomato sauce, spicy foods, high-fat foods, fried foods, garlic and onions, caffeinated drinks, carbonated beverages, chocolate, peppermint, and dairy.
Eat fermented foods such as yogurt, kefir, kombucha, kimchi, and sauerkraut.
Eat enzyme-rich foods such as pineapples, papaya, banana, kiwi, apricot, and avocados.
When foods are eaten raw or lightly steamed more live natural enzymes are preserved
Fresh pressed fruit juices are a good source of enzymes but should be consumed shortly after extraction because natural plant enzymes break down quickly.
Eat fiber-rich foods like whole grains, fruits, and vegetables, chia seeds, flaxseeds, oatmeal, dates, and pears.
A high fiber diet increases both frequency and quantity of bowel movements, which can help prevent constipation and bloating which contribute to reflux.
Avoid food sensitivities, food allergies, and known trigger foods.
Eat smaller sized meals
Eat slowly
Chew well
Don’t overeat
Don’t eat less than 2 hours before bed
Supplement Considerations for Reflux
Betaine Hydrochloric acid (HCl)
Magnesium Citrate [11]
Lifestyle Considerations for Reflux
Maintain a healthy weight
Exercise 60 minutes/day
Wait at least 3 hours before laying down after eating
Speak with your child’s doctor or pharmacist to determine if any current medications are contributing to reflux.
DISCLAIMER: Before starting any supplement or medication, always consult with your healthcare provider to ensure it is a good fit for your child. Dosage can vary based on age, weight, gender, and current diet.
Reflux & Autism in the Research
Prevalence and Identification of Reflux in Children with Autism
In this study, parents completed a 17 item screening to determine if their children with autism had any of the common gastrointestinal disorders linked to autism.[7]
This screening method identified children having one or more of these disorders with a sensitivity of 84%, specificity of 43%, and a positive predictive value of 67%.
This screening tool could be helpful in identifying gastrointestinal concerns in children who are very young, non-verbal, or who have difficulty expressing the source of their pain.
This method of parental screening identified that roughly 30% of children with autism experience reflux.
Reflux and Irritability
Children with autism with reflux exhibited unexplained irritability more frequently (43% of the time) than those children with autism who did not have reflux (13% of the time).[1]
This study suggests that diagnosing and taking steps to improve reflux may be helpful in resolving irritability in children with autism.
-
[1] Wasilewska J, Klukowski M. Gastrointestinal symptoms and autism spectrum disorder: links and risks - a possible new overlap syndrome. Pediatric Health Med Ther. 2015;6:153-166. Published 2015 Sep 28. doi:10.2147/PHMT.S85717
[2] Horvath K, Perman JA. Autism and gastrointestinal symptoms. Curr Gastroenterol Rep. 2002;4(3):251–258.
[3] Acid Reflux: Q&A with GI Specialist Tim Buie. Autism Speaks. https://www.autismspeaks.org/expert-opinion/acid-reflux-qa-gi-specialist-tim-buie. Accessed September 30, 2021.
[4] Gastrointestinal (GI) Problems in Children with Autism. The Place for Children with Autism. https://theplaceforchildrenwithautism.com/autism-blog/gastrointestinal-gi-problems-in-children-with-autism. Published October 3, 2019. Accessed September 30, 2021.
[5] Heifert TA, Susi A, Hisle-Gorman E, et al. Feeding Disorders in Children With Autism Spectrum Disorders Are Associated With Eosinophilic Esophagitis. J Pediatr Gastroenterol Nutr. 2016;63(4):e69-e73. doi:10.1097/MPG.0000000000001282
[6] Denham JM, ed. Gastroesophageal Reflux (for Parents) - Nemours Kidshealth. KidsHealth. https://kidshealth.org/en/parents/gerd-reflux.html. Published January 2021. Accessed September 30, 2021.
[7] Margolis KG, Buie TM, Turner JB, et al. Development of a Brief Parent-Report Screen for Common Gastrointestinal Disorders in Autism Spectrum Disorder. J Autism Dev Disord. 2019;49(1):349-362. doi:10.1007/s10803-018-3767-7
[8] Baird DC, Harker DJ, Karmes AS. Diagnosis and Treatment of Gastroesophageal Reflux in Infants and Children. Am Fam Physician. 2015;92(8):705-714.
[9] McElhanon B, Sharp, Karpen S, McCracken C. Gastrointestinal symptoms in autism spectrum disorder: A meta-analysis. Pediatrics. https://pubmed.ncbi.nlm.nih.gov/24777214/. Accessed October 2021.
[10] Madra M, Ringel R, Margolis KG. Gastrointestinal issues and autism spectrum disorder. Child and adolescent psychiatric clinics of North America. https://pubmed.ncbi.nlm.nih.gov/32471598/. Accessed October 2021.
[11] Neiworth-Petshow EM, Baldwin-Sayre C. Naturopathic Treatment of Gastrointestinal Dysfunction in the Setting of Parkinson's Disease. Integr Med (Encinitas). 2018;17(4):44-50.
Authors
Brittyn Coleman, MS, RDN/LD, CLT
Sinead Adedipe, MS