Constipation
What is Constipation?
Constipation is typically defined as having dry, hard stools with generally fewer than 3 bowel movements per week. Constipation often causes pain and straining while toileting, stomach discomfort, and bloating. It can be chronic (long-term) or can occur just once in a while. It’s estimated that up to 30% of all kids experience constipation across the world [1]. For children on the autism spectrum, research studies show us that constipation is the most common gut symptom and may affect up to 85% of this population [2, 3, 4, 5, 6, 7]. It’s also increasingly recognized that gut issues may contribute to feeding issues & picky eating in autism [2, 8]
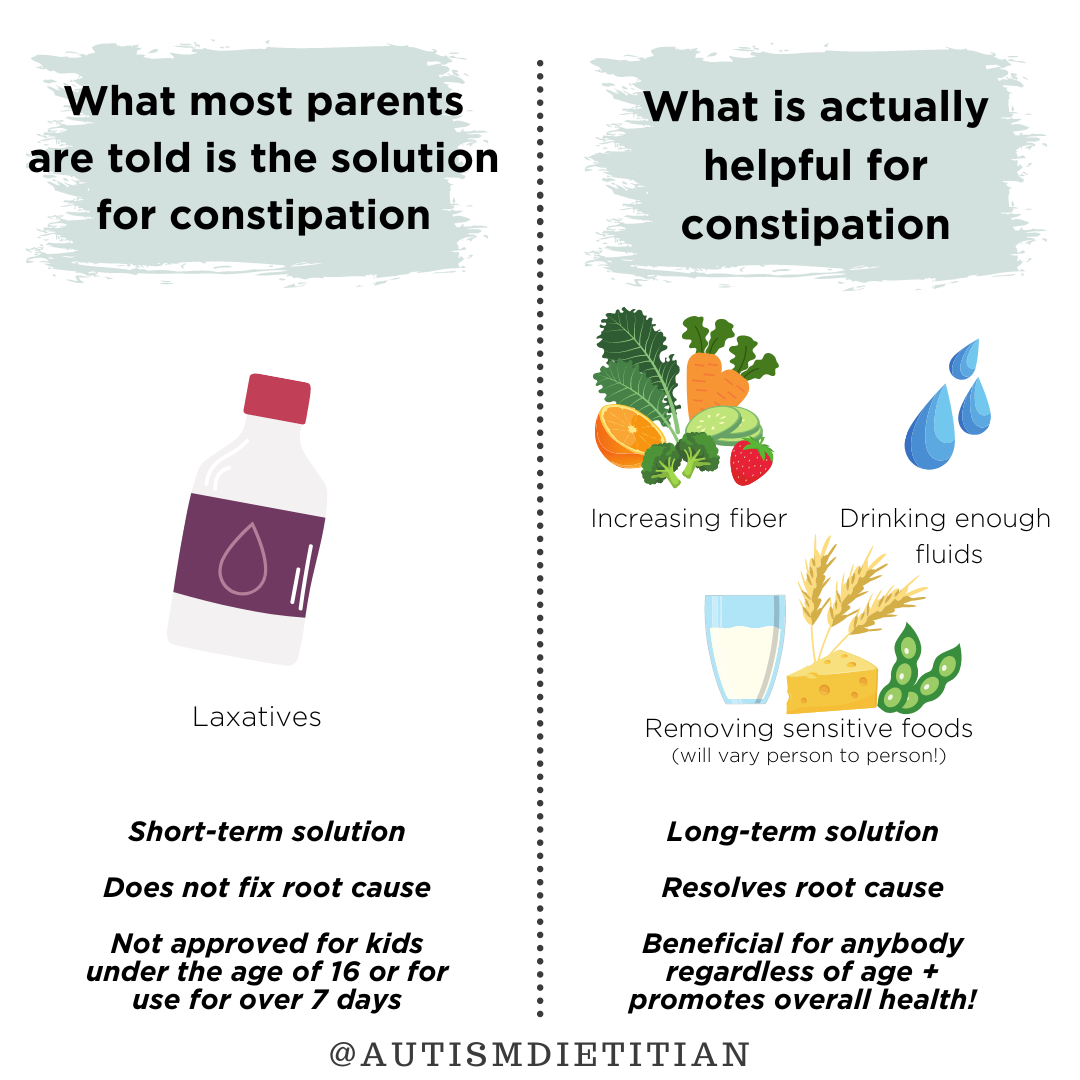
The most commonly prescribed treatment for constipation is over-the-counter laxatives (such as Miralax), that more serves as a “bandaid” and not actually a long-term solution to the underlying problem. Many individuals are surprised to learn that Miralax is not FDA approved for use for longer than 1 week or for use in children under 16 years of age (read the label here).
Chronic constipation can lead to an enlarged colon and a condition called encopresis, which is the involuntary leakage of stool. This can seem like the individual struggles with diarrhea, although it is actually stemming from constipation.
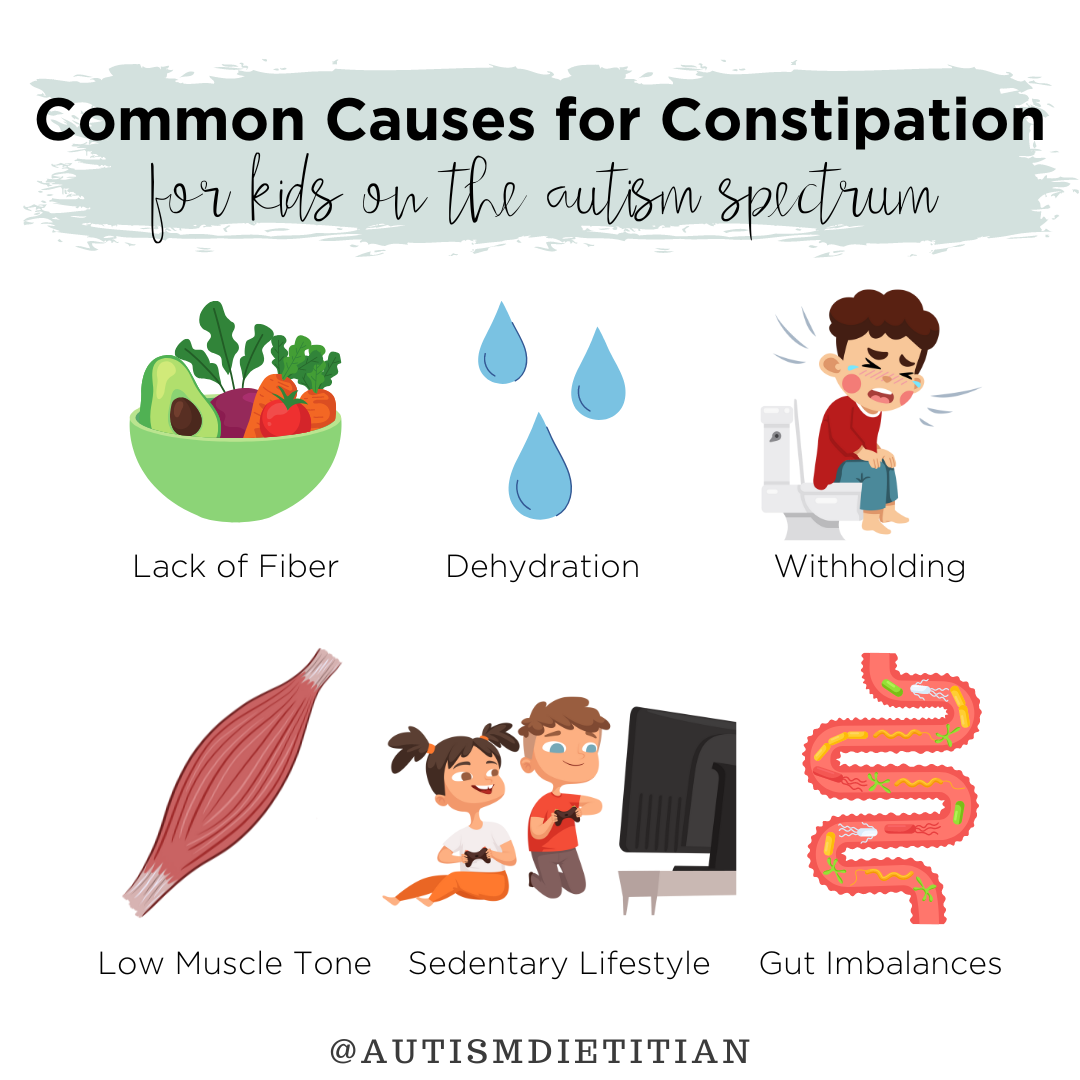
Potential Root Causes
The cause of constipation can be straightforward, or it can be more complex. Two of the most common reasons for constipation in children include dehydration and not consuming enough fiber. If your child is a picky eater, this could also be a large contributing factor to constipation.
For kids on the autism spectrum, withholding can be a common cause of constipation. They often withhold stool due to the unfavorable sensory experience of passing a bowel movement. Unfortunately, the longer a stool is withheld, the larger and harder the stool becomes, making it more and more difficult to pass, leading to even more withholding.
Other factors that affect constipation include (but are not limited to) a sedentary lifestyle, low muscle tone, certain medications, food sensitivities, imbalance of the gut bacteria (dysbiosis), and yeast overgrowth [9, 10]. If you suspect any of these factors, it’s best to consult with a functional medicine practitioner to help you run lab testing and create a protocol individualized to your child.
Constipation & Autism
Constipation is consistently reported as the most common gastrointestinal symptom in autism. Interestingly, research shows that the more severe the gastrointestinal problems, the more autism symptoms increase (including social impairment and verbal ability) [11, 12, 13]. Constipation can also negatively impact sleep, mood, and anxiety.
Constipation may be overlooked in children with autism, potentially because they may not be able to communicate that they are experiencing this issue. Atypical behaviors to look for that could indicate constipation include self-abusive behavior, posturing (such as bending over furniture) grimacing, holding the abdomen, squeezing the legs together, walking around with a narrow gait to hold stool in, constant eating or drinking, and chewing on non-edible objects. [14, 15]
Constipation is a common cause for picky eating and food selectivity in autism [16]. It’s not uncommon then for a child’s picky eating to contribute to more constipation, which then further impacts picky eating. This can often lead to a snowball effect that creates both severe constipation and extreme picky eating. Addressing gastrointestinal issues and imbalances can be the first step to break this cycle.
BOTTOM LINE:
Constipation is the most common gastrointestinal symptom for individuals on the autism spectrum and is correlated to increased autism symptoms and picky eating. Addressing the underlying reason(s) for constipation can resolve these issues long-term and greatly improve the child’s wellbeing and comfort.
Resolving Constipation
Diet
Make sure your child is getting enough fiber in their diet! If not, focus on high fiber foods like fruits, vegetables, beans/lentils, and whole grains
Certain foods can especially help with constipation including apples, pears, kiwi, oatmeal, prunes, ground flaxseed, soaked chia seeds, berries, and beans.
Hydrate, hydrate, hydrate! Kids should drink the number of 8 ounce cups of water equal to their age, up to 8 cups. For example, a child who is 3 years old should generally drink 3 cups (24 fluid ounces), a child who is 5 years old should generally drink 5 cups (40 fluid ounces), and children 8 and up should drink 8 cups (64 fluid ounces).
Consider if food sensitivities may be contributing to constipation. Dairy and gluten are the most common, but a child can theoretically be sensitive to any food. Please note that a food allergy panel will not show a food sensitivity. A proper elimination diet or food sensitivity testing with a functional medicine practitioner can help target specific foods that may be contributing.
Please note: if your child is an extreme picky eater, please do not remove any of their safe foods until you consult a feeding therapist.
Supplements
If your child isn’t getting enough fiber in their diet, consider a prebiotic supplement
Magnesium, specifically magnesium citrate, is a natural laxative and can make BMs easier to pass
Natural CALM makes powders and gummies that are easy for kids to take! We’ve found these products to be rather gentle on the GI system, but may not be enough support for some kids (everyone has different tolerances)
For a stronger product, we like OmniBlue Ocean Minerals. The dosages recommended by OmniBlue are:
Infants and Children: Safe, approved by Moms Across America. Always introduce progressively and verify tolerance. Everyone's metabolism and GI tract is different.
Children ages 1-3 years : 12 drops spread out through the day
Children ages 4-8: 8-15 drops spread out through the day
Pre-Teen: 20 drops spread out throughout the day
Teens: Integrate gradually starting from a quarter teaspoon up to a teaspoon in at least three to four days.
Adults: Integrate gradually starting from a quarter teaspoon up to one and a half teaspoon in at least three to four days.
Epsom salt baths (magnesium sulfate salts) can help with relaxation of the muscles and can also encourage a bowel movement
Probiotics can help add beneficial bacteria to the gut to encourage healthy bowel movements [17]. Certain strains may be more beneficial in relieving constipation, such as Lactobacillus casei, reuteri, & acidophilus and Bifidobacterium breve, bifidum, longum, & infantis.
MCT Oil can serve as a natural laxative
Did you know that certain iron supplements can cause constipation? In particular, iron supplements often cause harder stools.
Lifestyle/Other
The CDC recommends that children ages 3-5 should be physically active throughout the entirety of the day, and children and adolescents ages 6-17 require 60 minutes or more of moderate-to-vigorous physical activity daily. [18]
Consider if any of the medications your child is taking could be contributing to constipation. Discuss with your doctor before changing or stopping any medications.
Setting a consistent toileting routine for your child can help with regular bowel movements, especially if your child often doesn’t get the sensation to have a bowel movement
Research if Pediatric Pelvic Floor Physical Therapy could be beneficial for your child. You may also consider discussing toileting with your child’s Occupational Therapist or Physical Therapist.
Try abdominal massage to help promote a bowel movement [19]. Use the “I Love U” technique. Watch a video here.
Regularly visiting a chiropractor can also encourage healthy bowel movements [20]
DISCLAIMER: Before starting any supplement or medication, always consult with your healthcare provider to ensure it is a good fit for your child. Dosage can vary based on age, weight, gender, and current diet.
Authors
Written by: Brittyn Coleman & Elisa Rocks, RDN
Edited & Reviewed by: Brittyn Coleman, MS, RDN/LD, CLT