PANS & PANDAS
What are PANS & PANDAS?
PANS and PANDAS are autoimmune conditions when an infectious disease, environmental factors, and other possible triggers create a misdirected immune response that results in inflammation on a child’s brain.[1] PANDAS stands for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections. PANS stands for Pediatric Acute-onset Neuropsychiatric Syndrome and can be triggered by many factors and infections, including Lyme disease, mononucleosis, mycoplasma, and even the flu [1,5] Both are often seen in pediatrics , beginning around age 3 up until puberty, and most cases go away into adulthood.
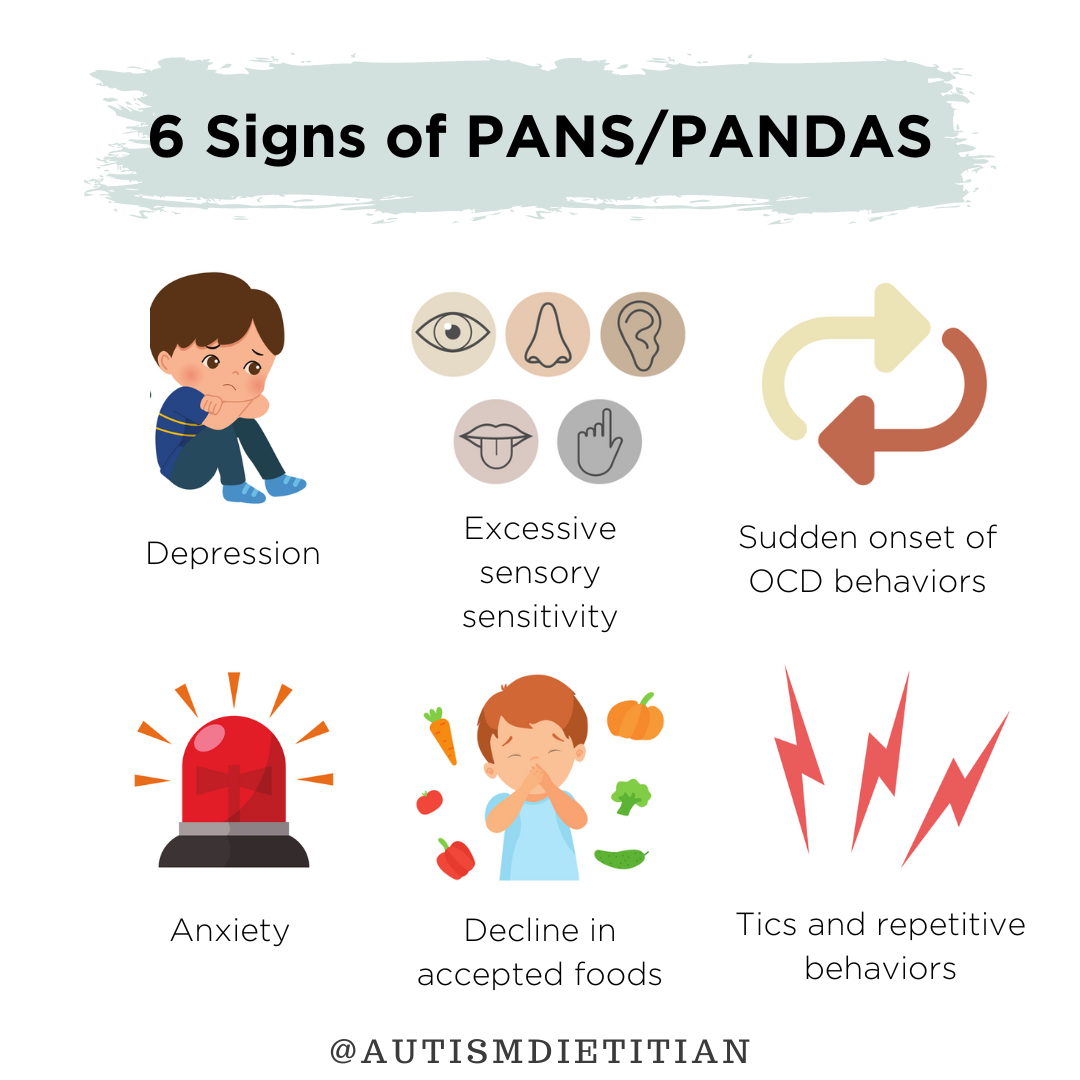
Both PANS and PANDAS can cause children to exhibit sudden, life-changing symptoms including OCD symptoms, tics, anxiety, sensory sensitivities, restrictive eating, a deterioration in school performance, changes in handwriting, bedwetting, mood swings, aggression, depression, oppositional defiance, developmental regressions, and sleep disturbances. [1] These symptoms typically reach full-scale intensity within 24-48 hours. [5] Neurologists believe that PANS/PANDAS affect the basal ganglia of the brain and have even been considered being renamed “Basal Ganglia Encephalitis” by some. The PANDAS Network estimates that PANS and PANDAS affect as many as 1 in 200 children [2]
PANS, PANDAS & Autism
There is currently no research on the prevalence of PANS/PANDAS in children with autism. As far as we know, the prevalence rate is not higher in autism than among other children. There can be overlapping symptoms between autism and PANS/PANDAS, which may make it harder to diagnose. Autism Speaks also mentions that it may be mistaken for classic OCD, which commonly co-occurs with autism. [6] Both autism and PANS/PANDAS involve neuroinflammation and immune dysfunction.[8]
There is some research that suggests that an imbalanced gut microbiome (dysbiosis) is at the root of both autism and PANS/PANDAS. According to one review, several studies also suggest a relationship between the presence of obsessive-compulsive disorders like PANDAS and alterations to the gut microbiota. [9] Another study found that streptococcal infections alter gut bacteria and cause inflammation and activate an immune response. [11]
Another study showed that children affected by PANDAS have high circulating levels of LPS (aka lipopolysaccharide, which is associated with neuroinflammation). The high serum levels of zonulin in PANDAS patients suggest that gut permeability (leaky gut) is enhanced in this neuropsychiatric disorder and may also contribute to the inflammatory LPS. [13]
A third study looked at a case of a 16 year old, who was diagnosed with PANDAS at age 12. After implementing the GAPS diet for 18 months, the child’s symptoms were gone and his immune function labs had all returned to normal levels. He lost his PANDAS diagnosis and was able to come off his medications. [10] The GAPS diet is largely focused on healing GI damage which then leads to improvements in brain function.
BOTTOM LINE
PANS/PANDAS and autism can have symptoms that look quite similar. If you suspect your child has PANS or PANDAS, work with a provider to explore your concerns and determine if testing is appropriate so you can take appropriate action to help your child.
Testing for PANS/PANDAS
There are a few tests that you can ask your physician to run to help give some more answers as to what may be causing a PANS/PANDAS flare, but there is not currently a 100% definitive test for PANS or PANDAS. The following is a list from the PANDAS Network for recommended bloodwork. Click here for more information on testing.
Basic Blood Work
IgE Level
IgA, IgM,
IgG (subclass 1, 2, 3, 4)
CBC
ANA
Ferritin
B-12
Vitamin D
Additional Testing
Cunningham Panel* – autoimmune autoantibody levels: Dopamine D1 receptor, Dopamine D2L receptor, Lysoganglioside GM1, Tubulin, & CaM Kinase II. Read more about the panel.
Viral/Bacterial Testing
Strep throat culture
Antistreptolysin O (ASO)
Anti dNase B
Streptozyme
Lyme Disease and co-infections
Mycoplasma Pneumoniae IgA & IgM
Pneumococcal Antibody Titers
Epstein Barr Virus Panel
Coxsackie A & B Titers
HHV-6 Titers
Medical Treatment for PANS/PANDAS
The most common approach used for PANS and PANDAS is antibiotics, though the type of antibiotic will vary based on the type of infection. Common antibiotics include Penicillin, Augmentin, Cephalosporins, and Azithromycin. It’s important to consider the implications of antibiotic use, especially long-term antibiotic implications.
Antibiotics should not be used without the guidance of a licensed physician and should not be stopped before the full dose is finished or when the child’s symptoms “start going away”. Stopping a round of antibiotics prior to the full protocol may cause antibiotic resistance. Some physicians will use long-term prophylactic antibiotics - meaning that they use it as a preventative measure over multiple months.
It’s important to remember that antibiotics not only kill off the bad bacteria but also wipe out the good bacteria in our gastrointestinal system. If using antibiotics, it’s essential to support the gut in other ways to ensure a healthy microbiome balance. While antibiotics are a true modern medicine miracle, they should be used sparingly and not without cause.
Other medical treatments used by other clinicians include IVIG, Plasmapheris, Ibuprofen, Cognitive Behavioral Therapy (CBT), Steroids, Tonsillectomy (tonsil removal), and Fecal Microbiota Transplant (FMT). For more about some of these treatments, visit the PANDAS Network [4]. For nutrition-focused approaches, please see “Next Steps” below.
Next Steps
Diet
Focus on whole foods including fruits, vegetables, protein, whole grains, and healthy fats that are naturally nutrient-dense (contain lots of vitamins and minerals) and fiber to support the gut (especially if using an antibiotic).
Reduce processed and “junk” foods containing added sugars and artificial ingredients as much as possible to support gut health and reduce inflammatory foods. This can also prevent yeast overgrowth or dysbiosis after using an antibiotic.
Reduce inflammation by avoiding foods causing any food reactions (allergies, sensitivities, intolerances, etc.)
The most common foods include dairy, gluten, sugar, and artificial ingredients/chemicals.
Focus on foods with omega-3s (i.e. fatty fish, ground flax, chia seeds, etc.)
Consider seasoning food with anti-inflammatory herbs such as turmeric/curcumin, ginger, oregano, and peppermint.
Focus on foods containing nutrients that support the immune system including vitamin C, zinc, and vitamin A.
Some anecdotal evidence suggests trialing camel milk or donkey milk as a potential treatment for PANS/PANDAS.
Consider reducing foods with high amounts of histamines in the child’s diet including fermented foods (like cheese and aged meats),avocado, dried fruits, leftover foods, tomatoes, vinegars, yeast products, etc.
Supplements
Take probiotics to provide the gut with beneficial bacteria that can help promote gut function and immune response. If using an antibiotic, a probiotic is a necessity, though should be taken at a minimum of 2 hours apart from an antibiotic.
Consider increasing intake of omega-3s through supplements (i.e. fish oil), as they are anti-inflammatory and are known for their positive effects on the brain.
Supplement with vitamin D, as vitamin D deficiency may be more common in PANDAS [7]
If not using antibiotics, consider antimicrobial herbals including Grapefruit Seed Extract, Olive Leaf Extract, Oil of Oregano, Garlic Extract, Caprylic Acid, Undecylenic acid, Berberine, MCT Oil, Goldenseal, Tea Tree Oil, etc.
We love using herbal combinations, such as Biocidin. One round of treatment often lasts 2-3 months, and depending on the person, it may take 1-3 rounds.
Ensure adequate nutrient levels of immune-supporting nutrients by supplementing with vitamins and minerals such as vitamin C, zinc, and vitamin A.
If the child becomes more sensitive to histamines, consider a probiotic that blocks histamine or this histamine blocker (see Nutritional Considerations above for more information about histamine foods)
Other supplements may be helpful based on the symptoms the child is experiencing. For example, lemon balm, L-theanine or magnesium may be helpful for anxiety or sleep disturbances.
Lifestyle
Practice and teach proper hygiene and handwashing to avoid or reduce exposure to Streptococcus or other illnesses.
Get 15-20 minutes of sun exposure each day. Vitamin D is an important nutrient for the immune system, and is best absorbed via the skin through direct sunlight.
Consider reducing environmental toxins to reduce toxic load, which may reduce inflammation and promote a healthy immune system.
Enroll in Cognitive Behavioral Therapy (CBT), which can significantly help the child and family with managing OCD symptoms, cope with stress, and address behaviors.
DISCLAIMER: Before starting any supplement or medication, always consult with your healthcare provider to ensure it is a good fit for your child. Dosage can vary based on age, weight, gender, and current diet.