Hypotonia (Low Muscle Tone)
What is Hypotonia?
Hypotonia is the medical term for decreased muscle tone, in which the muscle always seems to be relaxed, which makes coordinating movements difficult. This can lead to underuse and muscle weakness.[1]
Low muscle tone (sometimes called “low tone”) can affect the entire body including the muscles of the face and the digestive tract which may cause constipation or reduced motility. Because movement is difficult, those with hypotonia may tend towards being sedentary which also contributes to constipation.
Hypotonia is typically diagnosed by a neurologist after a variety of tests have been done to determine the root cause.
Therapies like occupational, physical, and speech/language therapy are often recommended and can help manage or improve the condition. [1]
One study noted that hypotonia is prevalent in those with mitochondrial disease, those with ASD and mitochondrial disease, and those only with ASD. [3, 5]
A recent study found that 34% of children with ASD had generalized hypotonia.[7]
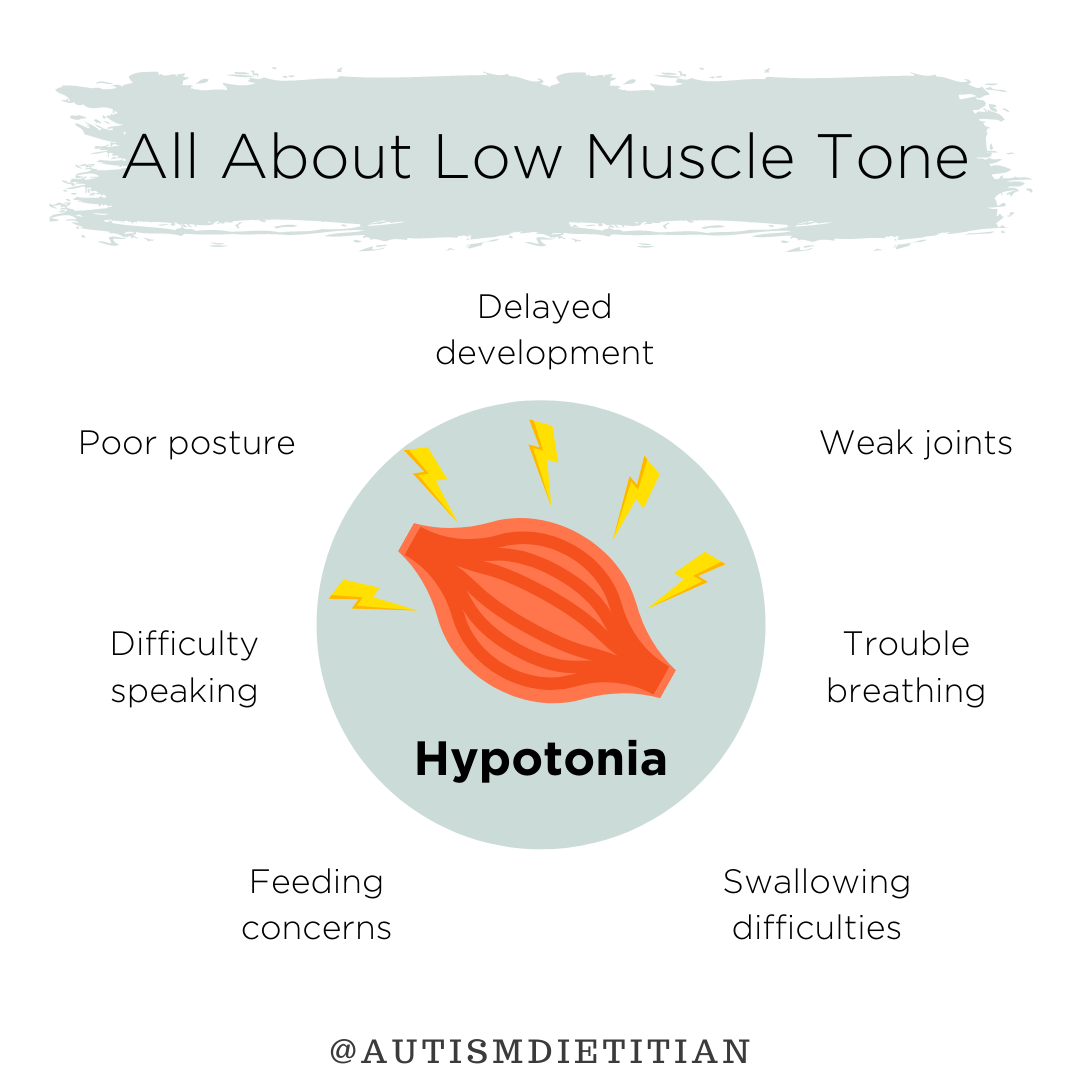
Signs & Symptoms
Symptoms of hypotonia include: [1,2]
Delayed developmental milestones
Poor posture
Infants may appear floppy
Trouble breathing or speaking
Difficulty chewing/swallowing, which could cause feeding issues
Laxity of the joints with dislocation or hyperextension
Poor reflexes
Contributing Factors
Hypotonia can be a symptom of an underlying condition such as mitochondrial dysfunction or be caused by damage to the central nervous system (brain and spinal cord). [3]
Damage can result from trauma, environmental factors, or genetic, muscle, or central nervous system disorders like autism, Down syndrome, muscular dystrophy, Prader-Willi syndrome etc.[2]
The Chromosome 2q37 Deletion Syndrome is a rare genetic disease characterized by short stature, hypotonia, intellectual disability and developmental delay. About 25% of people with this condition also have ASD. [8,10]
Next Steps
Diet
Children with hypotonia may be picky eaters and prefer foods (especially carbohydrates) that dissolve in the mouth or are easy to chew. A high carbohydrate diet may result in blood sugar levels that dramatically rise and fall throughout the day. Balancing meals and snacks with protein, fat, and fiber can help stabilize blood sugar.
Protein-rich foods like beef, chicken, and fish are good sources of carnitine and CoQ10. Deficiencies in these could result in hypotonia and/or mitochondrial dysfunction.
It is important to determine if the child is getting adequate calories, especially if they tire quickly while eating or have difficulty chewing, swallowing, or supporting their torso and head while eating. There may be nutrient deficiencies if the child refuses entire food groups due to limited ability to chew or swallow.
A child with chewing or swallowing limitations may need their food or fluids to be thickened to avoid choking or aspiration. This can be evaluated by a speech-language pathologist.
Fiber and water should be prioritized considering the tendency toward constipation in those with hypotonia.
Hypotonia in the muscles of the mouth may make it difficult for an infant or child to make a seal with their lips in order to drink. Ensuring a child’s fluids needs are being met is all the more important.
Optimizing the health of the mitochondria is important. This can be done by reducing toxins in the diet and the home environment, resolving any nutrient deficiencies and prioritizing antioxidants and anti-inflammatory foods.
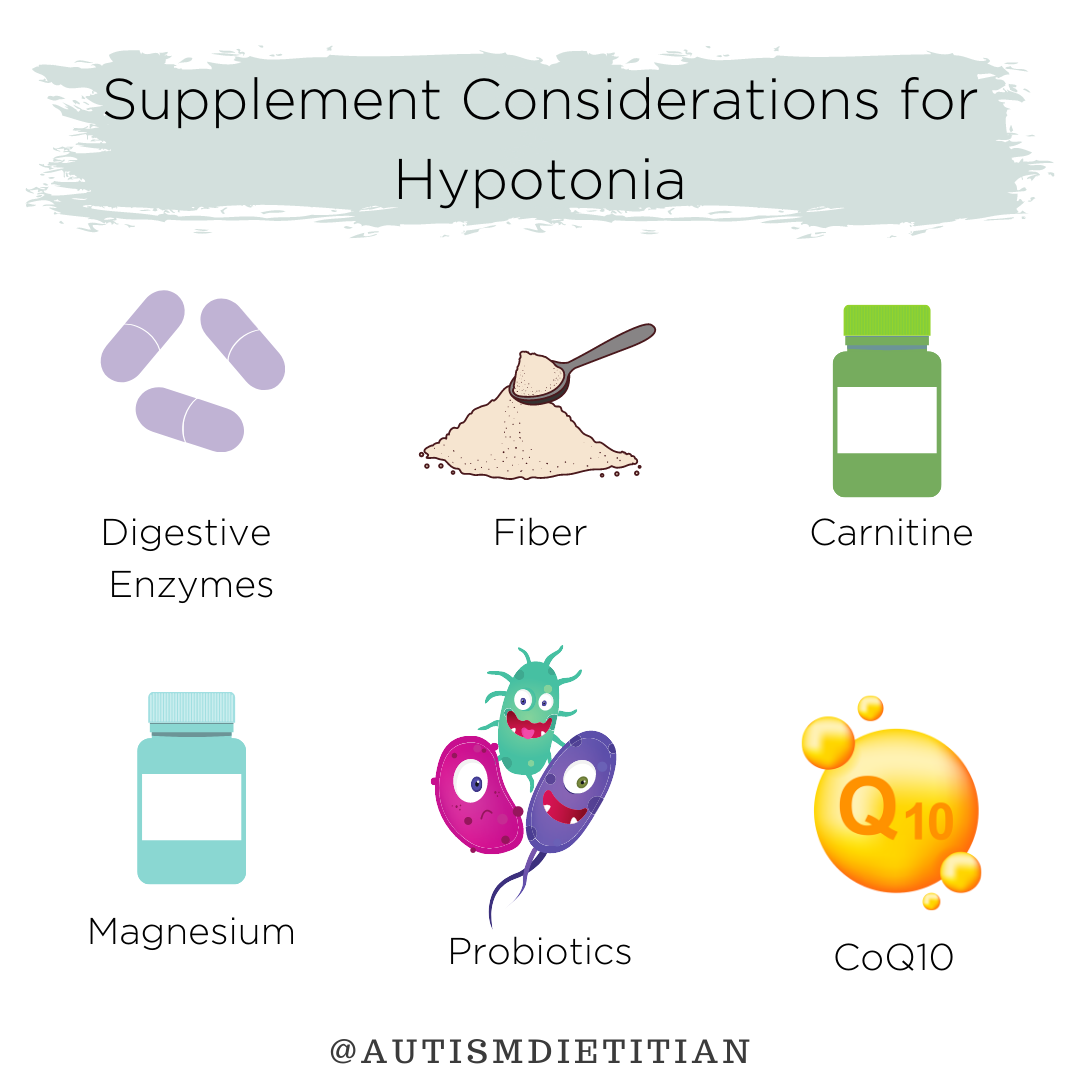
Supplements
Supplements for constipation may be beneficial including fiber, magnesium, MCT oil, and probiotics.
Digestive enzymes may aid in the breakdown of foods that have not been chewed thoroughly.
Carnitine and Coenzyme Q10 supplements are beneficial for those with hypotonia, ASD and mitochondrial dysfunction.
Lifestyle
As mentioned above, early intervention with appropriate therapies can help manage or treat/improve hypotonia and mitigate developmental delays and other symptoms associated with hypotonia.
Occupational therapists can help children perform activities of daily living, including gross and fine motor skills like drinking from a cup or using feeding utensils.
Speech/language pathologists can help determine if a child has difficulties with chewing or swallowing and how best to address those challenges. They can also help a child with speech development.
Physical therapists can provide exercise recommendations to help strengthen the muscles and make overall movement easier.
DISCLAIMER: Before starting any supplement or medication, always consult with your healthcare provider to ensure it is a good fit for your child. Dosage can vary based on age, weight, gender, and current diet.
Hypotonia & Autism in the Research
Hypotonia & Mitochondrial Dysfunction
Our findings suggest that mitochondrial dysfunction may be present in children with a clinical constellation including hypotonia, epileptic seizures, autism, and developmental delay. [4]
Hypotonia & Autism Diagnosis
Hypotonia is a recognizable marker of ASD and may serve as a "red flag" to prompt earlier recognition and neurodevelopmental evaluation toward an autism diagnosis.[6]
Hypotonia is associated with other motor abnormalities and could be an early marker for higher autistic symptom severity and lower quality of life in young children with ASD. [7]
Muscle hypotonia is associated with higher autistic symptom severity and lower quality of life in children with ASD. Children with ASD and muscle hypotonia have more common motor stereotypies and a later onset of independent walking. [7]
Hypotonia was the most common motor symptom in our ASD cohort (51%) and this appeared to improve over time, as suggested by the significant reduction in prevalence in older children. [9]
Hypotonia & Carnitine
Two conditions, in which hypotonia is a common symptom are Prader-Willi syndrome (PWS) and Down syndrome. Individuals with PWS had higher serum levels of carnitine esters and higher ester-to-free carnitine ratios than controls suggesting a possible underlying impairment of peripheral carnitine utilization and mitochondrial energy metabolism in some individuals with PWS. [11]
Carnitine deficiency or coenzyme Q10 (CoQ10) deficiency may present with hypotonia, poor growth, easy fatigability, and apnea. [11]
Carnitine level was significantly lower in Down syndrome patients compared with normal children between 6 months to 5 years of age. [12]
-
[1] Hypotonia information page. Nih.gov. https://www.ninds.nih.gov/Disorders/All-Disorders/Hypotonia-Information-Page. Accessed December 16, 2021.
[2] Muscle Weakness (Hypotonia). Childrenshospital.org. https://www.childrenshospital.org/conditions-and-treatments/conditions/m/muscle-weakness-hypotonia. Accessed December 16, 2021.
[3] Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Mol Psychiatry. 2012;17(3):290-314.
[4] Fillano JJ, Goldenthal MJ, Rhodes CH, Marín-García J. Mitochondrial dysfunction in patients with hypotonia, epilepsy, autism, and developmental delay: HEADD syndrome. J Child Neurol. 2002;17(6):435-9.
[5] Mitochondrial disease clinical manifestations: An overview. Bcmj.org. https://bcmj.org/articles/mitochondrial-disease-clinical-manifestations-overview. Accessed December 16, 2021.
[6] Gabis LV, Shaham M, Leon Attia O, et al. The Weak Link: Hypotonia in Infancy and Autism Early Identification. Front Neurol. 2021;12:612674.
[7] Lopez-Espejo MA, Nuñez AC, Moscoso OC, Escobar RG. Clinical characteristics of children affected by autism spectrum disorder with and without generalized hypotonia. Eur J Pediatr. 2021;180(10):3243-6.
[8] Baeza-Velasco C, Cohen D, Hamonet C, et al. Autism, Joint Hypermobility-Related Disorders and Pain. Front Psychiatry. 2018;9:656.
[9] Ming X, Brimacombe M, Wagner GC. Prevalence of motor impairment in autism spectrum disorders. Brain Dev. 2007;29(9):565-70.
[10] 2q37 deletion syndrome. Medlineplus.gov. https://medlineplus.gov/genetics/condition/2q37-deletion-syndrome/. Accessed December 17, 2021.
[11] Miller JL, Lynn CH, Shuster J, Driscoll DJ. Carnitine and coenzyme Q10 levels in individuals with Prader-Willi syndrome. Am J Med Genet A. 2011;155A(3):569-73.
[12] Seven M, Cengiz M, Tüzgen S, Iscan MY. Plasma carnitine levels in children with Down syndrome. Am J Hum Biol. 2001;13(6):721-5.