Calcium
What is Calcium?
Calcium is an important mineral to build and maintain strong bones. Calcium also supports your heart, muscles, and nerves.
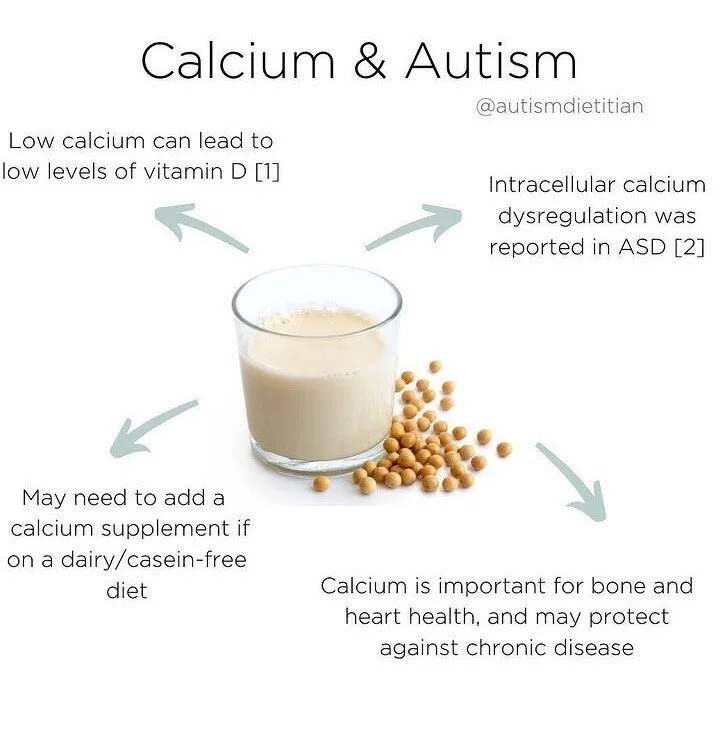
Due to restrictive diets, some children with autism may be at high risk for low calcium intake.
Most of the calcium in our bodies is held in our bones and teeth for structure, though a very small amount of calcium is used to benefit your blood vessels, muscles, nerves and hormones.
Bones undergo continuous breakdown and remodeling, which makes Calcium constantly needed. Serum Calcium does not fluctuate with dietary intake and will remain constant by pulling from stores in our bones.
Children with autism are more likely to have calcium deficiency than typically developing children, which makes nutrition evaluation and treatment an important step for many. [1-2]
Some treatments for individuals with autism include restrictive diets (ex. gluten free, casein-free) which raises concerns for inadequate intake of nutrients including calcium. [3]
Vitamin D intake and serum levels are important to increase calcium absorption. High intake of iron may decrease absorption of calcium.
Food Sources of Calcium
Dairy products
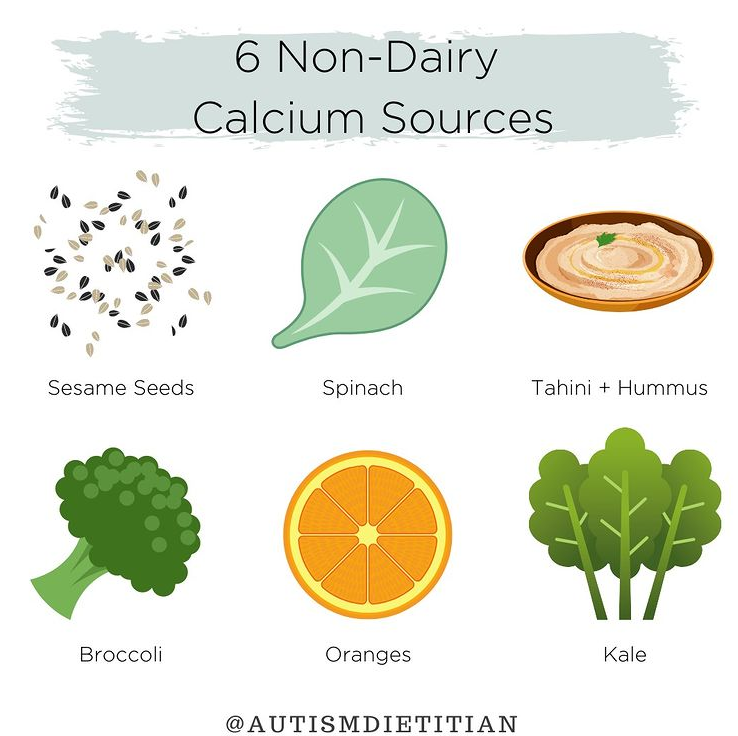
Non-dairy food sources
Milk alternatives fortified with calcium
Tip: Ripple Milk (pea milk) has the most similar amount to cow’s milk!
Fortified orange juice
Green leafy vegetables (like kale, spinach, collard greens, and arugula)
Broccoli
Fish where you eat the bones (such as sardines)
Soy products (soy milk, tofu, edamame)
Okra
Recommended Intake
These recommendations are based on the Recommended Dietary Allowance (RDA), which is the average daily level of intake sufficient to meet the nutrient recommendations of nearly all (97-98%) of healthy individuals.
Males & Females
1-3 years: 700 mg
4-8 years: 1000 mg
9-18 years: 1300 mg
19-70 years: 1000 mg
70+ years: 1200 mg
Deficiency
Dietary calcium deficiency has no obvious signs or symptoms in the short term. Long-term effects can include osteopenia and eventually osteoporosis which will lead to an increased risk of bone fractures in older age.
Calcium deficiencies are often caused by medical conditions including renal failure, removal of the stomach, and medications like diuretics. Calcium levels could also be depleted in children who are picky eaters and do not consume any calcium sources or supplements.
Symptoms include…
Tingling fingers
Muscle cramps
Convulsions
Lethargy
Poor appetite
Abnormal heart rhythms.
Individuals at Higher Risk for Calcium Deficiency…
Children on certain medications such as PPI’s, SSRI’s, and anti-epileptic drugs
Individuals on a casein-free diets
Children with restricted diet
Lactose intolerance or cow’s milk allergy
Vegetarians or vegans
Postmenopausal women
Amenorrheic women (women without a period).
Toxicity
High levels of calcium can cause hypercalcemia commonly caused by thyroid imbalances or cancer. High levels of calcium can lead to:
GI upset (such as constipation)
Kidney issues
Cardiovascular issues (soft tissue calcification)
Calcium in the urine
Kidney stones
The Tolerable Upper Intake Level (UL) is the maximum daily intake unlikely to cause adverse health effects.
Males & Females
1-8 years: 2500 mg
9-18 years: 3000 mg
19-50 years: 2500 mg
51+ years: 2000 mg
Supplements
Calcium Carbonate is more available and less expensive. It is dependent on stomach acid to be absorbed, so it is best taken with food.
Calcium Citrate can be taken with or without food which makes it helpful for those with low stomach acid, inflammatory bowel disease, or absorption issues.
Calcium Gluconate and Lactate can also be found in supplement forms, but are not the best sources for calcium.
Calcium can also be found in over-the-counter antacid products like Tums® and Rolaids®.
Examples
Note: All supplements are linked to Amazon for convenience, however, buying supplements on Amazon does not guarantee quality, as there are many “unverified resellers” selling nutrition supplements. To buy supplements that are verified to be sent directly to the consumer, you can create an account on the Autism Dietitian FullScript and search for the respective supplement under “Catalog”.
DISCLAIMER: Before starting any supplement or medication, always consult with your healthcare provider to ensure it is a good fit for your child. Dosage can vary based on age, weight, gender, and current diet.
Calcium & Autism in the Research
Calcium Deficiency
Children with autism are more likely to have calcium deficiency than typically developing children, which makes nutrition evaluation and treatment an important step for many. [1-2]
Selective Eating
Some treatments for individuals with autism include restrictive diets (ex. gluten free, casein-free) which raises concerns for inadequate intake of nutrients including calcium. [3]
Children with autism are more likely to have feeding difficulties, restricting the variety of foods that are eaten, which can lead to deficiencies like calcium deficiency or even rickets. [4-5]
Bone Health
Children with autism are at a higher risk for low bone density which could lead to higher risks of fractures. This is connected to decreased exercise, restrictive diets low in calcium, and certain medications. [3,6]
Increased protein and calcium intake is associated positively with bone density values for boys with autism. [6]
-
[1] Shahjadi, S., Khan, A. S., Ahmed, M. U., Karim, M., Parvin, S., Siddiqi, U. R., Afroz, S., & Mahruba, S. N. (2020). Study On Serum Magnesium, Calcium And Iron In Autism Spectrum Disorder (ASD) Children. Journal of Dhaka Medical College, 27(2), 199-204. https://doi.org/10.3329/jdmc.v27i2.45834
[2] Guo M, Li L, Zhang Q, et al. Vitamin and mineral status of children with autism spectrum disorder in Hainan Province of China: associations with symptoms. Nutr Neurosci. 10.1080/1028415X.2018.1558762
[3] Shylaja Srinivasan, Julia O’Rourke, Sara Bersche Golas, Ann Neumeyer, Madhusmita Misra, "Calcium and Vitamin D Supplement Prescribing Practices among Providers Caring for Children with Autism Spectrum Disorders: Are We Addressing Bone Health?", Autism Research and Treatment, vol. 2016, Article ID 6763205, 6 pages, 2016. https://doi.org/10.1155/2016/6763205
[4] Tripathi N, Shankar RK, Baghdassarian A. Nutritional Rickets Presenting as Chronic Episodic Extremity Pain in a 9-year-old with Autism. Clin Pract Cases Emerg Med. 2018;2(3):251-254.
[5] Marí-bauset S, Llopis-gonzález A, Zazpe I, Marí-sanchis A, Morales suárez-varela M. Comparison of nutritional status between children with autism spectrum disorder and typically developing children in the Mediterranean Region (Valencia, Spain). Autism. 2017;21(3):310-322.
[6] Neumeyer AM, Cano sokoloff N, Mcdonnell EI, et al. Nutrition and Bone Density in Boys with Autism Spectrum Disorder. J Acad Nutr Diet. 2018;118(5):865-877.